December 1, 2009
The Canadian Institutes of Health Research (CIHR), Canada’s government agency responsible for funding health research, has awarded UBC Dentistry periodontal researchers funding for two investigations. Drs. Hannu Larjava and Lari Hakkinen will receive over $1.28 million combined over four- and five-years respectively to investigate enamel calcification, and scar formation.
Dr. Hannu Larjava Awarded Research Grant to Study Calcification of Enamel

Dr. Hannu Larjava
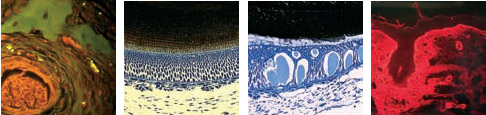
Just over $599,000 has been allocated over four-years for Dr. Hannu Larjava for his research titled “Critical role for alpha-v-beta-6 integrin in enamel biomineralization.” Enamel, notes Larjava, is the hardest mineralized tissue in the human body. It covers the crowns of teeth and protects the teeth from decay and functional wear during chewing and grinding the teeth together. It is the only calcified tissue in the body that is produced by epithelial-derived cells called ameloblasts.
During enamel formation, ameloblasts produce and process extracellular matrix that then becomes calcified to form fully mineralized enamel. A number of proteins that are crucially important for enamel formation have been discovered. Human mutations in some of these proteins cause inherited conditions in which enamel is poorly developed or calcified (called Amelogenesis Imperfecta; AI). Larjava points out that this can lead to extensive wear and decay in both the primary and permanent dentition. “Often, patients with AI lose their teeth at a young age or need to go through extensive restorative work to protect teeth from decay and attrition,” he says.
Larjava and his research team have recently discovered that mice lacking ameloblast surface protein alpha-v-beta-6 integrin show weakly calcified rough enamel that poorly resists wear during chewing. This integrin regulates cell adhesion to proteins that have an arginine-glycine-aspartic acid (RGD) amino acid motif but its function in ameloblasts is not known. In this grant proposal, Larjava will characterize in detail the enamel defect caused by alpha-v-beta-6 integrin deficiency and investigate the molecular mechanism by which alpha-v-beta-6 integrin regulates calcification of enamel. Larjava explains the optimism of his research: “Understanding the molecular mechanism of enamel calcification would help us not only to better diagnose genetic and acquired conditions that affect enamel formation and prevent destruction of crowns of teeth but also facilitate future endeavours aimed at tooth regeneration.”
Dr. Lari Hakkinen Receives Five-Year Research Grant Totalling $685k to Study the Molecular Mechanisms in Scar Formation
Scar formation following injury to skin is a common, unwanted outcome of the wound healing process. Clinically, scars can range from fine lines to expansive, disfiguring hypertrophic or keloid scars. Dr. Lari Hakkinen explains: “Regardless of the type of scars, they lead to considerable psychosocial impacts or physical complications or both for the individuals.” Furthermore he notes that at least 45 million patients in the United States alone undergo procedures that could benefit from therapies that reduce scar formation, resulting in a $4 billion anti-scarring therapy market annually.
Dr. Lari Hakkinen
During the last decades, using various animal models, steady progress has been made to identify factors that may reduce scar formation. In spite of these advances, no effective therapy to prevent scar formation exists today. This is likely because information from the animal models cannot always be applied to humans. Thus, better models to compare scar-free and scar-forming wound healing are needed. “Intriguingly, there is a common impression among clinicians that human oral mucosal wounds heal with minimal scar formation. However, there has been no rigorous experimental evidence that support this notion,” Hakkinen says.
Systematical studies of experimental wound healing in humans are, however, difficult to perform for ethical reasons. Hakkinen and his research team have, therefore, developed a red Duroc pig model. Skin wound healing in these pigs has been extensively characterized and closely resembles human skin wound healing and results in abnormal scar formation. They have shown that wounds in the oral mucosa of these animals heal with significantly reduced scar formation compared to skin wounds. “We have also confirmed that oral mucosal wound healing in these pigs is similar to that in human oral mucosa,” he says. “By using this model, we will identify novel mechanisms that promote scarless healing and reduce scar formation”. Hakkinen and his team believe that the present study will provide novel information that can be used to design therapies to reduce scar formation in human skin.